Get Relief From Acute Pancreatitis Now! Follow Our Simple Guide.
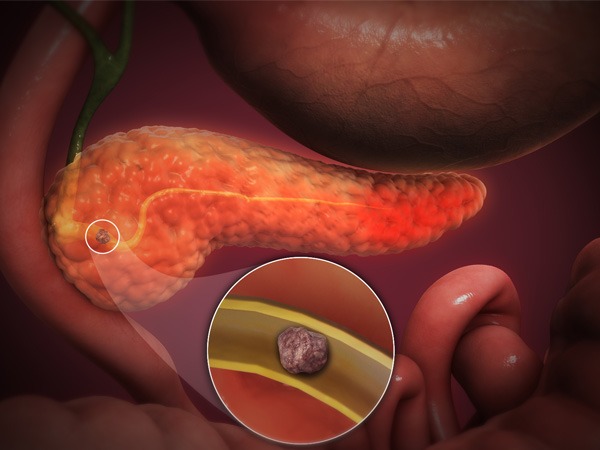
Acute Pancreatitis (AP) is an inflammation of the pancreas. It occurs when the pancreas becomes inflamed due to injury or infection. AP may result in severe pain in the upper abdomen, nausea, vomiting, loss of appetite, and jaundice. The cause of acute pancreatitis is unknown. However, gallstones, alcohol abuse, hyperlipidemia, trauma, drugs, and infections have been implicated as possible causes.
The risk of developing AP increases with age, especially after 50 years old. Other factors that increase the risk of AP include alcohol consumption, smoking, obesity, gallstones, diabetes mellitus, hyperlipidemia, trauma, and certain medications.
In the United States, the incidence rate of AP is estimated at approximately 30 per 100,000 people each year. However, the actual number of cases is likely much higher due to underreporting. In fact, many patients do not seek treatment for their symptoms until they have reached a critical stage of disease progression.
According to the National Institute of Diabetes and Digestive and Kidney Diseases, the mortality rate of AP is about 5% to 10%. Risk factors associated with increased mortality include older age, female gender, elevated serum creatinine levels, biliary tract obstruction, and systemic inflammatory response syndrome.
The causes of acute pancreatitis are varied. There are many different potential causes of acute pancreatitis including alcohol consumption, gallstones, excessive consumption of fatty foods (especially fast food), certain medications, autoimmune disease, trauma, hyperlipidemia, hereditary disorders, and infections.
Let us look at the various symptoms of Acute Pancreatitis
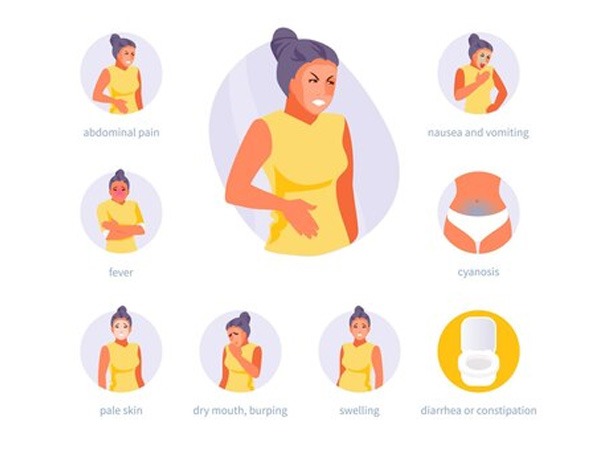
In mild cases, patients may recover completely with no long-term effects. However, if the inflammation spreads beyond the pancreas, it can lead to serious complications such as necrosis, infection, and fluid collection inside the body. If left untreated, these conditions may result in death. Below are the various symptoms of AP:
- Abdominal pain: The first symptom of acute pancreatitis is abdominal pain. It may begin suddenly, or it may start gradually over several days or weeks. The pain may feel like severe stomach cramps, a sharp stabbing pain, or pressure or tightness in the upper abdomen. It may spread to the back, shoulders, arms, neck, jaw, or legs. Pain may occur anywhere in the digestive tract, including the mouth, throat, esophagus, stomach, small intestine, colon, rectum, anus, bladder, or vagina.
- Nausea/vomiting: Nausea and vomiting are common symptoms of acute pancreatitis. These symptoms often start soon after the pain begins. Vomiting may happen at any time, even while sleeping. Sometimes people vomit only once, sometimes they vomit repeatedly. Vomiting may last for hours or days. If someone vomits repeatedly, he or she may have diarrhea (passing of loose stools) at the same time.
- Jaundice: Jaundice occurs when the liver becomes yellowish due to increased levels of bilirubin. Red blood cells break down to produce bilirubin, a pigment. When the body cannot get rid of bilirubin fast enough, it builds up in the bloodstream and causes jaundice. People who have had acute pancreatitis may develop jaundice.
- Fatigue: Fatigue is a feeling of extreme tiredness. It is not unusual for people with acute pancreatitis to feel extremely tired. Many people do not realize how much their bodies need rest until they have acute pancreatitis.
- Loss of appetite: Loss of appetite is another common symptom of acute pancreatitis. A person may lose interest in eating food, especially fatty foods. He or she may eat less than usual.
- Fever: Fever is a sign of infection. In some cases, fever may be caused by acute pancreatitis.
- Diarrhea: Diarrhea is the frequent passage of liquid stool. Usually, diarrhea happens early in the course of acute pancreatitis. Diarrhea may be watery or bloody. Bloody diarrhea means that the person has lost a lot of blood.
Diagnosis of Acute Pancreatitis

The diagnosis of AP is based on patient history, physical examination, laboratory tests, imaging studies, and endoscopic retrograde cholangiopancreatography (ERCP). Physical exam findings may include tenderness over the upper abdomen, rebound tenderness, jaundice, dark urine, and pale stool.
Laboratory testing may reveal elevated serum amylase and lipase levels. Imaging studies including computed tomography (CT), magnetic resonance cholangiopancreatography (MRCP), or ERCP may show a swollen pancreas, fluid collection around the pancreas, or narrowing of the ductal system. Endoscopy may identify changes in the appearance of the pancreas including swelling, edema, ulcerations, and necrosis.
Treatment options for Acute Pancreatitis

- Supportive Care: Supportive care is the first line of defense in treating acute pancreatitis. It includes fluid replacement, pain management, and nutritional support. Fluid replacement happens via intravenous (IV) fluids. You can do pain management with non-opioid analgesics and opioids. Nutrition support happens with enteral nutrition.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): Endoscopic retrograde cholangiopancreatogram (ERCP) is a procedure where a tube is inserted down the esophagus and into the stomach. If there is no blockage, the patient may receive medications to help prevent future attacks. If there is a blockage, the doctor may perform a sphincterotomy, which involves cutting away the area of the blockage.
- Antibiotics: You can use antibiotics to treat bacterial infections. However, antibiotics do not work well against viruses. In addition, they have side effects and may cause antibiotic-resistant bacteria. Therefore, they should be avoided unless absolutely necessary.
- Pancreatic Stent Placement: Pancreatic stents are placed to keep the duct open after ERCP. Stents come in two types: plastic and metal. Plastic stents are placed in the bile duct and remain in place permanently. Metal stents are placed in both the bile duct and pancreatic duct and stay in place only until they need replacing.
- Surgery: Surgery is performed if the patient’s condition does not improve with supportive care. In some cases, surgery may be necessary to remove parts of the pancreas or drain the pancreas.
- Treatment for gallstones: Gallbladder stones are formed from bile products. Gallstones are small, solid masses that may develop in the wall of the gallbladder. Gallstones can be cholesterol stones or pigment stones. A low-fat, vegetarian diet reduces gallstones. Avoiding fatty foods may help prevent gallstones.
When to seek emergency care?
Acute pancreatitis is a potentially fatal disease that happens through excessive production of digestive enzymes. The best way to avoid these complications is to recognize early symptoms and seek emergency treatment immediately. However, if you do not receive proper treatment soon enough, you may suffer serious consequences. Therefore, it’s important to know how to respond to pancreatitis symptoms.
How to treat pancreatitis at home?

If you experience mild symptoms of pancreatitis, you should continue eating and drinking normally to prevent dehydration. You might need to use over-the-counter medications to relieve symptoms. If you have moderate symptoms, you should drink plenty of fluids and take over-the-counter pain relievers to reduce discomfort. If you have severe symptoms, you should contact your doctor right away.
What to expect from your physician?
If you notice any symptoms of pancreatitis, call your primary care provider first before coming to the Emergency Department. Your doctor will likely perform tests to identify the cause of the condition and rule out other causes of similar symptoms. After testing, your doctor will determine whether you require hospitalization and what type of treatment you’ll receive while you’re there.
How long does pancreatitis last?
Pancreatitis may result in permanent damage to the pancreas. In some cases, however, symptoms may resolve spontaneously without further complications. The length of time it takes for symptoms to disappear after you have pancreatitis varies depending on the severity of the case. Generally, it takes two weeks for symptoms to go away completely.
What happens if I ignore my symptoms?
In rare instances, pancreatitis can lead to death if left untreated. Even if it doesn’t kill you, untreated pancreatitis makes recovery following surgery more difficult and increases the risk of gallstones, diabetes, and obesity later in life.
What is the diet for acute pancreatitis?
The diet for acute pancreatitis consists primarily of foods high in protein and fats. These types of foods help maintain blood sugar levels and prevent them from dropping. You should not take food that has carbohydrates as they increase insulin production, which may cause hypoglycemia (low blood sugar).
In the end,
Some people who have had AP do not experience any problems after their attacks. However, some people have repeated attacks and some people may die from AP. There is no way to predict who will develop AP again. However, risk factors may include heavy alcohol consumption, gallbladder disease, diabetes, hyperlipidemia, obesity, smoking cigarettes, certain drugs, trauma, surgery, and hereditary conditions.
If someone has AP, they should go to the hospital immediately. Treatment includes fluid replacement, analgesia, anti-emetics, antibiotics, and management of complications. A CT scan will rule out biliary tract obstruction. Once patients are stable, they should begin aggressive nutritional support including intravenous feeding via a central line and parenteral nutrition.
Frequently Asked Questions
What Does Pancreatitis Pain Feel Like?
The pain of pancreatitis varies but is often described as severe, persistent abdominal pain that may radiate to the back.
Do You Have Diarrhea With Pancreatitis?
Yes, pancreatitis can cause diarrhea due to poor absorption of fats and other nutrients.
What Does Pancreatic Cancer Poop Smell Like?
Faeces from pancreatic cancer may smell bad due to malabsorption caused by the tumor blocking the pancreatic ducts.
Does Pancreatitis Cause Constipation?
Pancreatitis can cause constipation because the production of pancreatic enzymes impairs digestion.
What are the Acute Pancreatitis Physical Exam Findings?
Physical examination findings in acute pancreatitis may include tenderness, resistance, and possibly abdominal distension.
Does Pancreatitis Cause Diarrhea?
Yes, diarrhea is a common symptom of pancreatitis and is often accompanied by abdominal pain and nausea.